
As the calendar turns to 2025, it’s a perfect opportunity to reflect, reset, and refocus. For those living with Parkinson’s—as well as the care partners and family members who support them—the new year offers a chance to set meaningful goals that prioritize health, wellness, and quality of life. Goal-setting can feel overwhelming, but breaking it down into practical steps can make all the difference. Here are some strategies to help you live well with Parkinson’s in 2025.
Harness the Power of Organization
Consistency is key when managing Parkinson’s. Start by organizing your day-to-day activities:
- Track medications and appointments: Use a planner or a dedicated app to ensure you never miss a dose or a check-up. Apps like Medisafe can help streamline this process.
- Plan ahead: Scheduling your week can create structure and reduce stress, especially when it comes to exercise, therapy sessions, or meal prep.
Set Realistic Goals
Achieving a big goal begins with small, manageable steps:
- Start small: Whether it’s incorporating a 10-minute daily walk or adding a new vegetable to your diet, incremental changes can build momentum and foster a sense of accomplishment.
- Celebrate progress: Acknowledge each milestone, no matter how small—it’s all part of the journey toward better health.
Prioritize Fitness
Exercise is a proven way to manage Parkinson’s symptoms, enhance mobility, and boost overall well-being:
- Explore Parkinson’s-friendly fitness programs: Look for activities like tai chi, yoga, or boxing programs like Rock Steady Boxing. These can improve balance, strength, and flexibility.
- Create a schedule: Consistency is vital. Even 15 minutes of daily movement can make a difference.
Focus on Nutrition
A balanced diet can help manage symptoms and maintain energy levels:
- Consult a professional: A dietitian familiar with Parkinson’s can tailor a plan to your needs, emphasizing brain-healthy foods like berries, nuts, and leafy greens. (check out our blog “Nutritional Super Stars for Parkinson’s)
- Stay hydrated: Dehydration can exacerbate symptoms, so keep water handy throughout the day.
Support Mental Health
Mental health is as important as physical health. Parkinson’s can sometimes lead to anxiety or depression, so proactive care is essential:
- Practice mindfulness or meditation: Techniques like deep breathing or mindfulness can help reduce stress and promote emotional balance.
- Seek connection: Whether through a support group or a regular coffee chat with a friend, staying connected can combat feelings of isolation.
Caregivers: Set Your Own Goals
Caregiving is an act of love, but it’s also demanding. Caregivers should set goals for their own self-care:
- Carve out “me time”: Whether it’s reading, walking, or pursuing a hobby, prioritize activities that recharge you.
- Join our Care Partners Support Group: Connecting with other caregivers can provide practical advice and emotional support. (email info@petersonforparkinsons.org for more information on meetings)
The Power of Goal-Setting in Parkinson’s Management 
Every goal, no matter how small, can be a step toward living well with Parkinson’s. As you map out your goals for 2025, remember that flexibility and self-compassion are key. Not every day will go as planned, but each effort contributes to your overall well-being.
Here’s to a year of progress, positivity, and purpose!


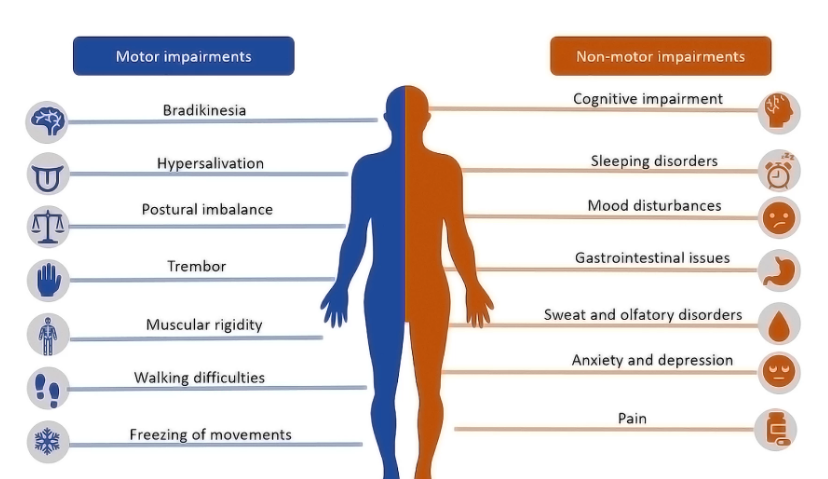
 When it comes to Parkinson’s Disease (PD), understanding and managing cognitive health is crucial for maintaining quality of life. During our recent Empowering Minds: Parkinson’s Mental Wellness for Patients, Families and Caregivers, Dr. Kaltra Dhima from Vanderbilt Medical Center, alongside MyLiveability Occupational Therapists Dr. Carlene Johnson OTD/OTR/L and Tori Vik shed light on the intricacies of cognition in PD and offered valuable strategies for maximizing long-term brain health.
When it comes to Parkinson’s Disease (PD), understanding and managing cognitive health is crucial for maintaining quality of life. During our recent Empowering Minds: Parkinson’s Mental Wellness for Patients, Families and Caregivers, Dr. Kaltra Dhima from Vanderbilt Medical Center, alongside MyLiveability Occupational Therapists Dr. Carlene Johnson OTD/OTR/L and Tori Vik shed light on the intricacies of cognition in PD and offered valuable strategies for maximizing long-term brain health.













 Pickleball, a sport that combines elements of tennis, badminton, and ping-pong, has gained recognition for its numerous benefits, particularly for individuals dealing with Parkinson’s disease. Several advantages of the sport include:
Pickleball, a sport that combines elements of tennis, badminton, and ping-pong, has gained recognition for its numerous benefits, particularly for individuals dealing with Parkinson’s disease. Several advantages of the sport include: The Pickleball group now thrives every Friday from 2:00 to 4:00 at the JCC, with the invaluable presence of Bo Sacks, a Senior Olympic winner and a top-ranked player in Tennessee. Bo brings not just expertise, but a patient and compassionate coaching approach tailored to individual skill levels.
The Pickleball group now thrives every Friday from 2:00 to 4:00 at the JCC, with the invaluable presence of Bo Sacks, a Senior Olympic winner and a top-ranked player in Tennessee. Bo brings not just expertise, but a patient and compassionate coaching approach tailored to individual skill levels.
 When it comes to fruits, blueberries are particularly beneficial for individuals with Parkinson’s. These small, antioxidant-rich berries offer a host of advantages.
When it comes to fruits, blueberries are particularly beneficial for individuals with Parkinson’s. These small, antioxidant-rich berries offer a host of advantages. individuals living with Parkinson’s disease. These vibrant greens are loaded with essential vitamins, minerals, and antioxidants that support brain health and overall well-being.
individuals living with Parkinson’s disease. These vibrant greens are loaded with essential vitamins, minerals, and antioxidants that support brain health and overall well-being. Citrus fruits like oranges, grapefruits, and lemons not only add a burst of flavor to your meals but also provide valuable benefits for individuals living with Parkinson’s disease. These brightly colored fruits are renowned for their high vitamin C content and other beneficial compounds.
Citrus fruits like oranges, grapefruits, and lemons not only add a burst of flavor to your meals but also provide valuable benefits for individuals living with Parkinson’s disease. These brightly colored fruits are renowned for their high vitamin C content and other beneficial compounds.

 For many, the holidays are a joyful time to gather with loved ones and friends, reflect on the past year and think about what’s to come. But for some with recently diagnosed or progressing Parkinson’s or with depression or anxiety, it can be a stressful or lonely time. Visiting with others can bring worry or increased symptoms, and not attending social events can bring feelings of isolation. These are natural and common reactions.
For many, the holidays are a joyful time to gather with loved ones and friends, reflect on the past year and think about what’s to come. But for some with recently diagnosed or progressing Parkinson’s or with depression or anxiety, it can be a stressful or lonely time. Visiting with others can bring worry or increased symptoms, and not attending social events can bring feelings of isolation. These are natural and common reactions.